HOME | ABOUT US | MEDIA KIT | CONTACT US | INQUIRE
HOME | ABOUT US | MEDIA KIT | CONTACT US | INQUIRE
Health--Care Executives Assess KC Preparedness, Response
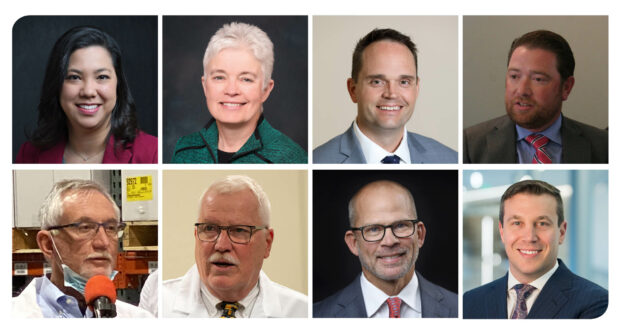
(Top row, left to right) Elizabeth Byrd, Lockton Companies; Melinda Estes, Saint Luke’s Health System; Sam Huenergardt, AdventHealth Shawnee Mission; Matt McInnes, McInnes Group. (Bottom row, left to right) Gary Morsch, Covid Care Force; Lee Norman, Kansas Department; of Health and Environment; Rich Reda, Lockton Companies; David Wild, The University of Kansas Health System.
In late March, a sign appeared in front of our AdventHealth Shawnee Mission’s medical Center in Merriam. It read, simply, “Heroes work here.” It was not, says the health system’s CEO, Sam Huenergardt, an exaggeration.
“This is unlike anything we’ve faced in modern history, and it will decimate the country unless we take it more seriously.” — Gary Morsch, founder, Covid Care Force
“We’re fighting a war against coronavirus and our caregivers are on the front line,” he says. “And don’t forget, it’s not just doctors and nurses. It’s everyone from the reception desk staff and respiratory therapists to the environmental services and nutritional-services teams.”
He was one of the top executives from the region’s leading health systems and health insurance providers asked to assess progress in the COVID-19 war, addressing everything from new collaborations to community support, from supply chain and safety needs of workers to lessons learned from other cities where the fight rages, barely under control.
Their responses are powerful reminders that the Kansas City region is blessed with an exceptional level of health care, both at the organizational level and the individual level of hands-on care.
A heart-warming development in the regional COVID-19 fight, health-care executives say, has been an unfettered community response showing support for the front-line workers providing care.
“We’ve seen in the outpouring of cards, signs, hand-made masks, donations of other supplies to help keep our teams safe, and so many other gestures of kindness and support just how much our community cares not only about what’s happening with this virus, but about the people who take care of their health,” said Melinda Estes, president and CEO of Saint Luke’s Health System.
“Our communities are listening to what we’re asking them to do,” Estes said. “We can see that in the numbers of cases at this point across our states and in our hospitals. And we simply can’t stop now. It’s going to be incredibly tempting as the weather gets warmer, we’ve been inside longer, and we—hopefully—see a continued downward trend in cases to tell ourselves, ‘it worked,’ and go back to our regular lifestyles.”
To that end, said physician Lee Norman, secretary of the Kansas Department of Health and Environment, people must understand how the threat around them changes when they are outside their homes. “If you were in church next to someone in a pew for an hour or more, that’s pretty intimate contact,” he said. “If you go past someone in a grocery store, that’s more like two ships passing in the night.”
Federal relief to states and medical facilities is critically important, but Norman pointed to some missing pieces. “We appreciate that Congress is getting us money, but what we really need is stuff—we need the supply chain. Rather than pulling random numbers from the air to measure spread, we want harder indicators, but don’t have the testing materials. We can forecast disease activity, but prominence? That’s not easy to measure, and when you talk about reopening the economy, if we can’t handle a bad outcome, we shouldn’t open it up. We’re pushing hard and fast to get materials, but at this point, it’s all supply chain.”
David Wild, a physician and vice president of performance improvement at the University of Kansas Hospital, said officials there were also dazzled by an outpouring of community support.
“We’ve had offers to help procure testing supplies from local business leaders, an enormous amount of food donated by local restaurants to keep our staff working on the front lines well fed, and we’ve had countless donations of supplies and PPE from churches, businesses, and individuals across our region,” Wild said. “All these things help remind each of us how much this amazing community is tackling this pandemic together.”
The effort can be enhanced, he said, by every individual resident of the region: “Reducing travel and physical contact as much as possible, wearing barrier masks (cloth or otherwise) when you absolutely can’t physically distance, and calling ahead if you have symptoms and think you need to be seen in an urgent care or emergency department are also things everyone can and should do.”
And there is more the public can do to step up, said Gary Morsch, founder of the physician volunteer group Covid Care Force.
“We have to be aggressive on public-health mitigation policies; they have to be enforced,” he said, during a break in his 12-hour shifts at a hospital in Queens, N.Y. “The message about being back in church for Easter, that was the wrong message. People hear that and this and think no big deal. I had a guy yesterday tell me that a good rain would wash the virus away, if you can believe that. This is unlike anything we’ve faced in modern history, and it will decimate the country unless we take it more seriously. It will require everything on every front to stop it. The bottom line is, all aspects of this are new, different and unknown,” he said.
Sam Huenergardt, CEO at AdventHealth Shawnee Mission, also sees more challenges ahead.
“The biggest help to hospitals and our teams on the front lines is to get our community to stay at home,” Huenergardt said. “We are seeing positive signs that the early stay at home orders issued throughout the region are having an impact.”
Huenergardt also called for better coordination around acquisition of personal-protection equipment for front-line health workers. “Issues where states and the federal government are outbidding each other on supplies aren’t helpful for anyone,” he said. “We need a stronger, coordinated approach.”
There are many ways to help health-care providers at this pivotal moment, said Matt McInnes, president and CEO of the McInnes Group, an insurance and benefits consultancy. Specifically, he said, the firm was advising clients to help keep provider offices and local hospitals as empty as possible, so they can concentrate on the influx of COVID-19 patients and muster the resources required to care for them. “This can be done relatively simply,” he said. “Stay home and while you are at home avoid activities that could potentially cause an accident. Bottom line BE CAREFUL, now is a time to be mindful of what you are doing and what could potentially happen.”
Employers must continue to keep their staff out of the office, if possible, by working remotely, he said, adding: “If you are blessed to be in a financially stable position, donate to our local hospitals.”
David Wild emphasized the need for people with other conditions to seek appropriate care and not feel that it is unsafe to seek it. “To help make sure everyone has access to the care they need, we’ve worked extremely hard to shorten the deployment of our telehealth platform from nearly two years down to a couple of weeks,” he said. “If you have health problems or concerns which require you to visit one of our clinics, it’s very likely we can now see you and provide a treatment plan via our telehealth platform.”
Staying on top of health-care needs, Wild said, even in such an unprecedented time, helps prevent urgent needs or hospitalizations down the road. Telehealth services have also proven welcome for older patients, even some in their 90s.
“In a time when we’re encouraging patients to stay at home unless it’s absolutely essential for them to go out, it’s still incredibly important for us to continue caring for their overall health,” Melinda Estes said.
For Saint Luke’s, that includes implementing virtual visits among many of its primary care and specialty clinics. “We’re evaluating when virtual visits are appropriate on a case-by-case basis and then reaching out to patients to transition upcoming appointments to virtual visits,” Estes said. “This is no small feat—one area of care alone has more than 5,000 visits being transitioned in the coming weeks.”
The health system has temporarily closed some of Convenient Care clinics and launched virtual visits with Convenient Care providers to continue caring for the same number of patients—including those with COVID-like symptoms who wouldn’t have been able to be seen in a clinic.
“Our providers have been extremely supportive of this use of technology and have adopted new processes seamlessly—and with the human connection and personalized touch, even from a distance, that are so important to us in the care we provide every day,” Estes said. “It makes me proud to see how everyone has worked together and supported one another to continue delivering our best to our patients in new ways.”
“In health care, learning from one another is always essential,” said Melinda Estes. She’s been part of conversations on the emerging threat since its earliest days, thanks to her role as chair of the Board of Trustees of the American Hospital Association.
“We saw early on what was happening on the coasts, and from the beginning have been ahead of the planning curve,” she said. “Preparing for not only the current situation we were experiencing—but the potential for what other parts of this country and the world were experiencing—we acted swiftly and strongly.”
Among those efforts: standing up a robust incident command, securing the supply chain, restricting visitation within all Saint Luke’s locations, and setting up employees to work from home where possible—an effort she attributed to being part of a national and global team. “We truly are all in this together,” Estes said.
Huenergardt said AdventHealth had benefitted from colleagues in hard hit areas, including New York, Florida and Louisiana.
“Those conversations have helped us navigate the decision-making to effectively avoid, to date, a significant health-delivery crisis,” he said. “It was amazing how quickly information from these areas was disseminated on the Web through professional medical societies, such as the American College of Emergency Medicine. At times, Facebook COVID physician groups have also provided us real-time lessons learned in the fight against this new enemy. This treasure trove of information has allowed us to develop novel ways to oxygenate our COVID patients. It’s allowed us to find safer ways to intubate those in respiratory failure. It’s allowed us to develop protocols for the administration of treatment medications currently under study. It’s allowed us to begin preserving our PPE at an earlier date so we don’t face critical shortages.”
For a disease that thrives on the interconnectedness of this world, Huenergardt said, “it’s that same connection that has been critical in our ability to fight it off, to keep our providers and patients safe, and to manage our operations to continue to serve both COVID-19 patients and the essential non-COVID needs of our community.”
In recent weeks, said David Wild, KU Health officials have conferred with, among others, physicians and healthcare leaders from China and Italy, Columbia University in New York City, and the University of Washington. Each of those conversations he said, “has helped us prepare in some way, and all of them have confirmed we are doing the right things to prepare very early on the curve. We’re participating in a number of clinical trials for treatments and preventative measures for healthcare workers who are exposed to a COVID-19 positive patient. All of these things are providing both hope and guidance as we continue to prepare.”
Caught in the grip of an unseen threat, “the health-care community has come together in some pretty amazing ways over the past few weeks,” said David Wild. “Leaders are meeting weekly, virtually of course, sharing current status and information about capacity, treatment efficacy, PPE guidelines, and emergency preparedness. This sharing helps us be better prepared and better able to support our community”
Those connections are being forged within and across organizations.
Sam Huenergardt said his incident command team has been meeting daily for nearly six weeks to coordinate responses, and the system draws on guidance from federal, state and county health departments, a well as the World Health Organization.
Collaborations also helped the hospital’s pathology group set up same-day testing protocols, he said. “That reduced the turnaround time for results from five to seven days to less than 12 hours. Further, the ongoing collaboration between the clinical pathologists, infectious disease specialists, pulmonologists, intensivists, hospitalists and other providers has allowed us to avoid pitfalls in testing that others have not been able to avoid.”
Executives at all levels share a common dread in this climate: A surge of patients that overwhelms the capacity of the regional delivery network—hence the ubiquitous references to curve-flattening. But capacity can be a concern in a number of areas.
“Some are physical, like the number of hospital beds or intensive care beds or the number of ventilators,” said David Wild. “Others are supply related, like the amount of gowns or N95 respirators or medications needed to provide care for critically ill patients. Some areas are worried about the number of health-care workers that are healthy and available to take care of patients.”
All are getting the health system’s attention, he said, but none is a critical concern at the moment, thanks in large part to individuals who have responded to calls for ensuring their own health.
“Part of the reason we haven’t seen a surge big enough to challenge capacity is the impact of physical distancing on reducing spread,” David Wild said. “It will be imperative in the next 60 days to continue to think differently about how we can re-engage in needed activities in a way that doesn’t increase the risk of spread due to increased physical contact. Just as we expanded telehealth rapidly, I’m sure there are ways other businesses and industries can use technology to meet the needs of their customers and our community and still protect each other and prevent a surge.”
And the fear extends to the safety of workers across those care systems.
“There’s no argument that the best way to prevent transmission of infection is to prevent contact with an infected person,” said Wild. “Health-care workers choose every day to take care of those who are sick, regardless of the cause of their illness. PPE, while not a substitute for limiting contact, is our best line of defense. If the number of patients needing care for COVID-19 were to increase, we will continue to do everything we can, including sourcing and disinfecting PPE in ways we might not have a month ago, to support our teams and keep them safe.”
Responding to reports that Google’s tracking systems had indicated an overall reduction of 30-40 percent in user movements though the region, David Wild said the numbers were encouraging.
“We know aggressive measures are likely needed to cease transmission–somewhere in the neighborhood of a reduction in interpersonal contact of 60-70 percent has been published,” Wild said. “What we don’t know is how a 30-40 percent reduction in cell phone movement relates to a percentage reduction in interpersonal contact. The number of hospitalizations in the next week or two will give us a much better picture of the impact of these reductions in movement.”
Health-care benefits, like the delivery of care itself, are undergoing fundamental change in front of our eyes.
“The distribution of health care will change forever” as a result of this crisis, Matt McInnes predicted. “Technology and virtual office visits will become the norm. Preventative care, frequent comprehensive blood testing, and precautionary screenings will become the centerpiece of benefit plans.”
That trend was naturally occurring, “but the recent events will greatly accelerate the movement towards this kind of medicine,” McInnes said. “It will affect and shape every employer’s total benefit package, meaning all aspects of their plan and how they work together. Medical insurance is the most obvious, but it will also transform disability and life insurance benefits significantly.”
In terms of costs, he said, preliminary research estimates that the total cost of medical claims will go up about 7 percent because of expenses associated with COVID-19. That means, he said, “self-funded and fully insured groups could receive this increase on top of trend factors and their own claims experience. There are many considerations that could potentially impact that number, but I do believe these preliminary findings will end up being relatively close as far as the cost associated with the virus.”
But he also believes that as health-care providers squeeze inefficiencies out of the system and people assume a renewed responsibility for their own health, “these factors could potentially offset or even outweigh the impact of COVID-19 costs. For the first time in decades, the short term cost of insurance claims could go down!”
Longer-term, McInnes said, he hopes Kansas City can start to return to normal life by June, but some parts of the nation could see stay-at-home orders extended in to early next year unless people get more serious about limiting outside contacts.
Elizabeth Byrd, vice president and Unit Leader for Lockton’s Healthcare Practice, works closely with clients on the impact of the virus and delivery of care. “The planning and diligence it takes to prepare for a pandemic of this size is remarkable,” she says. “We’ve seen clients enter new agreements quickly for supplies and materials, look to provide child care to ensure employees can come to work, lease temporary space to potentially move patients to free up hospital beds, sign up to conduct clinical trials, set up employee wellness hotlines, the list goes on. I’ve been most impressed with the number of volunteers, retirees, and providers currently in administrative roles reaching out and ready to help.”
The majority of the professional liability insurance carriers Lockton works with, she says, have been flexible and understanding of the immediate change in risk profiles that clients will assume.
“We are partnering with them to approve the rush requests and provide guidance when needed,” Byrd said. “The support of our community, business partners and governmental agencies will be vital for our healthcare clients to deliver the care our country needs.”
Her Lockton colleague, Rich Reda, is president of Benefit Communication Insourcing. Given the relatively low infection rate and even lower rate of patients requiring hospitalization, he said, “we do not expect significant pressure on medical costs directly attributable to COVID-19. However, health-care providers have had to set substantial portions of their caregivers on the sideline as ‘essential’ care is delivered. This has put tremendous margin pressure on all health systems.”
Government stimulus earmarked for these systems, will help, Reda said, “but it is too early to tell how much revenue and by extension margin can be recouped. We expect the cost of care and thus the cost of insuring employees may increase as a result in the coming months.”
Given what’s known now, there’s no way to determine whether Kansas City as a region is destined to experience New York’s fate, or whether it may dodge this bullet.
“This is very hard to predict,” said David Wild. “What we do know is the risk of spread will be present until there is a readily-available vaccine or treatment. With enough testing to identify pockets of infection before they become larger clusters of spread, there might be a way to safely relax some restrictions in the coming weeks, but it may be some time before all restrictions can be safely lifted.”
In the meantime, though, “we are finding hope every day, as we experience businesses caring for their employees,” Matt McInnes said. Across the firm’s hundreds of small-business clients, he said, “every one of them has been impacted by the pandemic. They are concerned about the toll this is taking on their business, but more than anything they are determined to help their employees.”
As for the care providers, said David Wild, “I think every health-care worker is driven at some level by a desire to serve others. There is some inherent risk every day in being a first responder or health-care worker, and we all love our work despite the risk. It’s sometimes harder
to wrap your head around the risk in situations like this- where there are un-knowns related to doing the work you are proud to do.”
He’s convinced, though, that “we are doing everything possible to ensure the safety of those on the front lines in our organization, as are countless others across the region. It’s possible doctors or nurses or first responders will be exposed in their work, and its possible some will
get sick. If they do, we’ll be here to take great care of them, too. It’s what we’re here for.”
Other unsung heroes, said Lee Norman, include state administrators working to organize supplies and delivery timetables, along with physicians like those he’s worked with at the National Guard.
“Inspiration happens every day in a crisis like this,” Norman said. “I’ve got people I’ve worked with for years, going back to H1N1 flu in 2009 and Ebola in 2014—it’s almost like getting the band back together again. It’s a different organism, but the mindset is ‘let’s get after it.’ It really brings out the best in people. It’s crisis communication at its best; the people I rely on are all-stars.”
Health care, declared Sam Huenergardt, “is sacred work. There hasn’t been another point in my lifetime where that has been clearer. We must do everything we possibly can to keep these heroes safe.”