HOME | ABOUT US | MEDIA KIT | CONTACT US | INQUIRE
HOME | ABOUT US | MEDIA KIT | CONTACT US | INQUIRE
The worst part of the 2020 pandemic has faded away, but health-care providers— and their patients—will feel the impact of that challenging time for years.
On May 11, just weeks from now, the Biden Administration will end a public-health emergency declaration issued more than three years ago as the pandemic swept the world. That same day, the Mid-America Regional Council’s daily online COVID-tracking hub will go dark after 1,153 days. America will be able to breathe easy knowing that, as Gerald Ford declared upon succeeding the scandalized Richard Nixon as president, “the long national nightmare is over.”
Or is it?
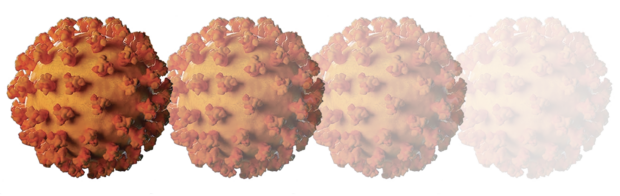
A virus credited with more than 1.06 million American deaths may no longer be raging at epidemic levels—not a single state health department reported COVID on April 9 in their preliminary reporting—but the virus that launched this scourge continues to morph into new variants. It always will. More contagious, perhaps, but if recent history is a guide, less lethal.
Still, the toll has been historic. Worldwide, more than 6.8 million deaths have been attributed to the virus in all its forms. Nearly 10 percent of the planet’s population is known to have been infected; estimates suggest it could be multiples of that. In the U.S., nearly 1.2 billion COVID tests were processed—an average of 3.5 per person—674 million vaccine doses have been administered, and more than 6 million people were hospitalized at some point since February 2020.
The cost of all that? Trillions. Not just for managing the health crisis and financing research and distribution of workable vaccines, but in lost workplace productivity, lost worker income, business failures, unpaid rent, lost life-years because of suicide, drug abuse, and deferred health-care delivery.
And, of course, a health-care delivery system rocked to its core and challenged in ways no living person can recall. An estimated 333,000 health-care workers, besieged with patient loads, quit their jobs in 2021 alone, according to one industry study. Worse, in 2021 alone, an estimated 3,600 health-care workers died after contracting the virus, many of them at work. That figure is more than 24 times the number of public-safety workers—police and firefighters—who died in the line of duty over that same year.
The path forward, health professionals say, offers reasons to be hopeful—and still too many reasons to be concerned.
“There is good news about where we are now with COVID-19,” says Lee Norman, former secretary of Health for Kansas and a past chief Medical Officer at The University of Kansas Hospital. For one, the virus is becoming more predictable in its behavior, which provides a better understanding of how to manage severe cases, he said. Lower transmission rates have allowed for the relaxation of anti-infective practices, such as mask-wearing and isolation.
The most encouraging, Norman says, is that the nation’s health-care system can take a fresh look at the care model. “Are there better models of team care that allow all providers to work better, at the top of their licenses, differently as a team, utilizing physicians, nurses, nurse practitioners, community health workers, and medical assistants?” he said. “Is that also true for (delivery of) care in homes and community locations, technology-assisted, as through telemedicine? I think yes.”
A primary concern for business is the long-term impacts that continue to dramatically reshape the workforce and the places where people used to work. The ability to work remotely has fundamentally changed recruiting and retention of talent for all business sectors—those whose workers can maintain productivity and those who find it harder to retain or recruit talent as more people insist on the flexibility of remote work.
The pandemic created new work-force challenges but also exacerbated—even sped up—trends in the workplace before the first U.S. COVID death. Remote and hybrid work may empty 330 million square feet of U.S. office space by 2030, according to a Cushman & Wakefield report earlier this year. With 740 million more square feet likely to become obsolete from non-pandemic trends, the nation is looking at a billion-square-foot office-space surplus within seven years.
Put in starker terms, that report warned that the 12 percent office vacancy rate of pre-pandemic 2019 could surge by more than half to 18 percent.
Lessons Learned—and Not
Looking back, Norman believes a clearer picture has emerged regarding opportunities lost amid the crisis response.
The notion that “science would carry the day was errant thinking,” he says. “Necessary and helpful, yes, but half of Americans chose not to believe or follow experts. On top of that, the speed of response was inadequate, exposing a disjointed nationwide patchwork of response frameworks and jurisdictional authorities.
Research findings—especially about masks—were often at odds with each other, further undermining public confidence, and political differences drowned out the voices of researchers, clinical experts, and public health authorities.
Political fault lines shifted further amid online conspiracy theories fomented by partisans of every stripe. It didn’t help boost confidence, for example, for candidate Joe Biden to declare weeks before the 2020 election that he couldn’t trust a vaccine produced during the Donald Trump administration, then flatly stated less than a year later that anyone who took the vaccine was “not going to get the virus, not gonna get sick and not gonna die.”
Looking back, the metrics would belie each of those claims.
Looking forward, health-care executives are hopeful that the pandemic response has generated momentum that can be sustained to improve messaging and processes for the next big danger lurking out there.
“It brought many federal, state, and county respondents together for the first time, and the partners oftentimes did work together well,” Norman said. “When a disaster occurs, it is not a great time to be exchanging business cards for the first time.”
Some good news: At this point in the viral cycle, the nation’s population generally has natural immunity as well as vaccine-induced immunity to COVID, said Dana Hawkinson, chief of infection control at The University of Kansas Hospital. A defensive posture looking down the road, he said, “continues to be about preparation and prevention—doing all these things to help prepare for new issues, but also prevention and testing and all that work on the front end. That will save you a lot on the back end.”
The nation will be better armed if another COVID variant hits, Hawkinson said, now that pharmaceutical companies have been able to roll out treatments that can be given at the onset of symptoms. Those have already proven they can vastly reduce the need for hospitalization, and in cases where hospital admission is required, stave off the worst of COVID’s effects.
“What we can do to prepare for the next pandemic,” Hawkinson said, “includes infrastructure for surveillance, resources to help research and development of new vaccines as well as potential therapeutics.”