| |
|
|
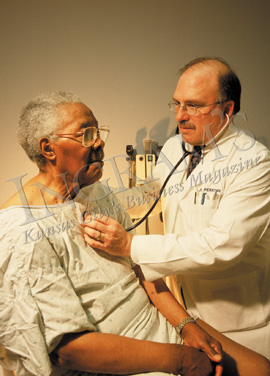
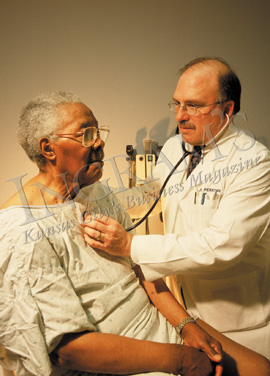
Gary
Berger
Physical Medicine & Rehabilitation
“Definitely a patient advocate who goes
above and beyond. He loves his patients and they love him.” These
glowing words were spoken about Dr. Gary Berger, D.O., who is Medical
Director, Rehabilitative Services for Menorah Medical Center as well as
Associate Medical Director for the Rehabilitation Institute.
Dr. Berger does agree that when he’s with his patients, they’re
all that matters. He chose rehabilitation as a specialty for the same
reason he chose his degree from Philadelphia College of Osteopathic Medicine:
it’s more hands-on, more comprehensive, and a more general practice
approach—a direction he says the medical profession has veered toward
since he graduated in 1983. He is rewarded by patients whom he helps to
recover their dignity, as they turn a disability into an impairment that
they can overcome. He believes there is great compensation when his patients
are able to regain their self-respect through what he and his staff have
taught them.
He points out the rehabilitation field is only about 60 years old, when
WWII made helping people adjust to physical change a necessity. Although
diagnostic testing has improved, and functional and assistive devices
of one kind or another have advanced, the real improvements have occurred
in understanding—for instance, a better understanding of stroke and
brain-damage recovery has helped better accommodate patients at home.
Outpatient care and resources have improved, so patients can leave the
hospital earlier and their families are encouraged to participate in the
process.
Dr. Berger left private practice in 1996—a good move, he says, because
now he has more freedom, camaraderie, and people to turn to with questions.
His passion in rehabilitative medicine has deepened even further to include
dealing with the effects of cancer, the disease his wife died of a year
ago. This has radically changed his life, he says, and that of his two
children, but in ways he would not have necessarily foreseen. “My
life is first with my kids. I’m both mom and dad — and I like
my life with them,” he explains quietly. “I wouldn’t have
it any other way.”
|
 |
|
Richard
Derman
OB/GYN
People who’ve served in the Peace Corps
always say they got more from it than they gave. Dr. Richard Derman wholeheartedly
agrees, for his pre-residency stint in India created his life’s direction.
Seeing the enormous trials and pains of the women in India led him to
become an ob-gyn and then to get a degree in public health from Johns
Hopkins.
From there, his life has been one filled with research as well as clinical
success. At the University of Illinois-Chicago, he helped create the comprehensive
program that received one of 15 federal designations as a Center of Excellence
in Women’s Health.
That work moved him to Kansas City when offered the commitment from both
Truman Medical Center and UMKC to use those successful models to create
a similar center for Kansas City. This will be a concentrated and seamless
continuum of care for women, made possible by the recent $1.3 million
grant from the Hall Family Foundation. “The idea is to link the expertise
at UMKC with clinical excellence and patient base at Truman. We will be
able to play a major role in women’s health care,” he enthuses.
Dr. Derman has the Schutte Chair in Medicine Leadership/Women’s Health
from Truman Medical Centers and UMKC, where he is professor as well as
associate dean. He is one of a handful of experts whose practice is limited
to menopause, but he has been involved in research in everything from
pelvic inflammatory disease to urinary pregnancy tests to alternative
medicine. He’s written a book on fertility control and edited one
on hormonal therapy.
He says others probably call him a workaholic, but he’s really very
people oriented. Dr. Derman notes that it’s funny how things come
round—he’s recently obtained another grant from the National
Institute of Health to prevent women hemorrhaging to death at childbirth—in
India. He loves each of the components of his work—patients, research,
and collaboration. “I’m very excited about the collaborative
effort I see going on in Kansas City. I hope to play an active role.”
Given his energy level and commitment, he surely will.
|
 |
|
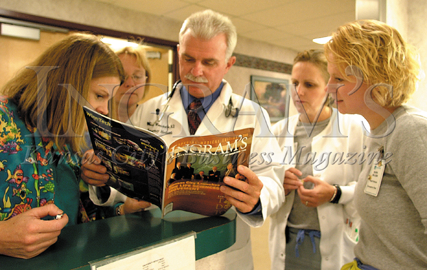
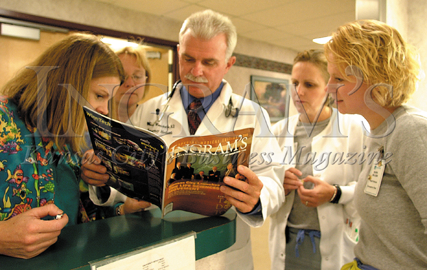
Mike
Johnston
Internist
“My wife and I were married in Oklahoma
at 2 p.m. on Saturday afternoon, graduated from college at 6 p.m. that
same day, drove to Kansas City on Sunday, and on Monday morning, I started
school at what’s now the University of Health Sciences, College of
Osteopathic Medicine. That was 32 years ago and I still owe her that honeymoon.”
Dr. Mike Johnston laughs as he thinks back to his start in the field that
he knew he wanted to be in because of his grandfather and uncle, both
of whom were physicians.
Perhaps considered a more holistic approach to healing, osteopathy heeds
the spiritual and mental well being of the patient as well as the physical.
Dr. Johnston is definitely a proponent of that approach and of his university
with its new educational pavilion and classroom facilities. His day is
spent with students, residents, and patients. He greatly enjoys his teaching
on the clinical side—”the passing on of my trade.” His
joy is apparently echoed by those he teaches—he’s received “Teacher
of the Year” five times within the past 10 years for both resident
and student teaching affiliated with UHS. And he goes this month to Orlando
to receive a national award, “Internist of the Year,” from the
American College of Osteopathic Internists at their annual meeting.
But what makes him most proud and happy, he says, is to be around a great
“house staff"—the doctors, interns, residents, and staff
people with whom he works on a daily basis. “I’m so very fortunate
to be surrounded by these people in this profession.”
Now chairman of the internal medicine department at UHS, professor, program
chair for internal medicine residency out of the Medical Center of Independence,
and general internist who still is in practice, Dr. Johnston truly enjoys
all aspects of his life—practicing medicine, mentoring and teaching.
“I tell my students it’s the greatest job in the world and it
comes from the left ventricle. There’s nothing more rewarding than
doing this work, but you have to love it, you must to have a passion for
it.”
Dr. Johnston has that passion.
|
 |
|
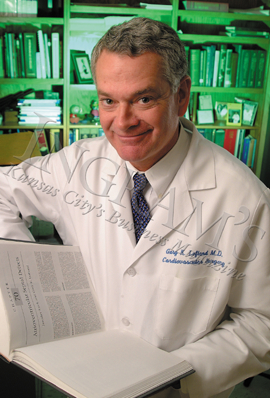
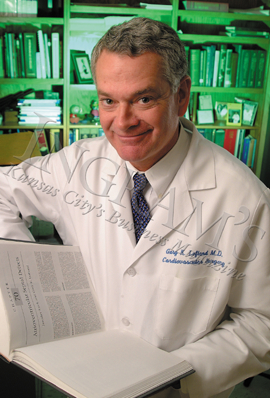
Gary
Lofland
Pediatric Cardiac Surgeon
You could probably bet that not many cardiothoracic
surgeons who specialize in congenital heart disease began their careers
on Indian reservations. But Gary Lofland, who always wanted to be a doctor,
encountered a couple of physicians while a resident at Duke University
Medical School who’d worked on reservations and recommended it. So
a young Dr. Lofland, not having defined his specialty yet, left for Montana
to run a medical center there as a primary-care physician. “It was
an amazing experience. I saw things there you wouldn’t see anywhere
except on a reservation . . . or in a third world country.”
But he left public health and went into research. He already knew he was
fascinated by surgery, especially thoracic surgery, and that attraction
led him to congenital heart disease. He thought such heart disease was
the most challenging to treat with surgery, and he still thinks so nearly
20 years later.
Dr. Lofland occupies the Joseph Boone Gregg chair at UMKC’s School
of Medicine and works more than full time for Children’s Mercy Hospital.
He operates on children as small as 450 grams up to full-sized adults
with congenital heart conditions. He works on a wide range of defects
and still finds it fascinating and rewarding. The children make up the
majority of his patients, and the most difficult thing about that, he
admits, is the emotional involvement and the extreme sense of responsibility
you feel for patients and families. “You are accepting responsibility
for an entire unlived lifetime,” Lofland says.
Doing over 500 operations a year leaves little time for hobbies—he
says his used to be “the lung"—but any free time is spent
with family, exercise, reading, or more sporadically, salt-water fishing
(“where anticipation of fishing is usually better than the fishing”).
He talks much more openly about the atmosphere and the people who create
it at Children’s Mercy, for they make a terribly risky and stress-filled
profession not just endurable, but actually fun.
“The culture starts at the top. We have highly skilled, wonderful
people here who have intelligence and joy. They share my enthusiasm. It’s
simply a great place to work.”
|
 |
|
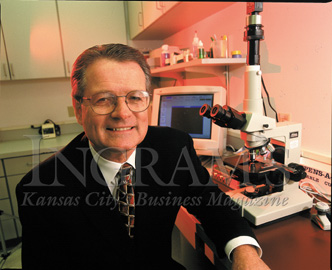
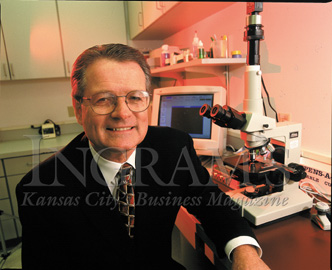
Rodney
Lyles
Reproductive Endocrinologist
“This is an art, not a science.”
So speaks Dr. Rodney Lyles about his work of creating babies from in vitro
fertilization and assisted reproductive technology. In 1988, when he founded
the Reproductive Resource Center in response to the fact that one married
couple in six confronts infertility, he knew that for half of infertile
couples, long-established medical treatment or surgical procedures could
successfully treat the problem. He wanted to work with the others.
His success rate has been remarkable, well above the national average
of 25 percent. Since the Overland Park center’s creation, there have
been over 5,000 babies born from all therapies, and over 1,600 babies
born as a result of assisted reproductive technology (ART). He attributes
that to his excellent lab, motivated donors, team approach, and the fact
that he gives couples all the information they need. “The worst thing
one can do is walk in here and say, ‘I want to be pregnant—do
whatever it takes.’ Since there are no guarantees, it’s our
job to give them all the information necessary so that they can make the
appropriate choice for themselves. That includes all the options, the
real success rates of live children born, the risks. Then they must decide,
not me.”
Dr. Lyles began as a gynecologist in Oklahoma, because he originally liked
working with a young, healthy group of people. He liked delivering babies.
Further study at Baylor College of Medicine in Houston in reproductive
endocrinology led him to an even greater satisfaction—helping people’s
dreams of having their own child come true. He speaks warmly of his staff’s
contribution to the process—”I’m fortunate to have such
a wonderful team who communicates very well and is so focused on what
we’re doing. We’ve been successful and busy because of that
focus we all share.”
He stresses that infertility programs and approaches vary widely, and
people must investigate thoroughly before they choose since it’s
expensive—and elective. “We want to absolutely do our best with
couples who couldn’t have children. If you’re in medicine, you’re
obligated to do the best you can.”
|
 |
|
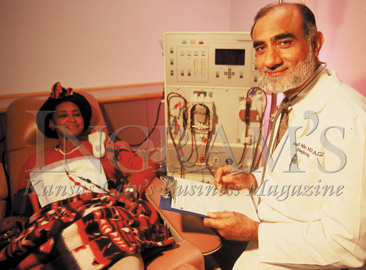
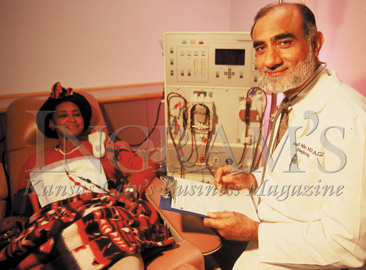
A. Rauf
Mir
Nephrologist
It was in 1972 when a young man from Kashmir
came to Trinity Lutheran Hospital to do an internship and residency in
internal medicine. He came with a couple of buddies; they were going to
do their residency, go back to Kashmir and open up a practice.
Thirty years later, Dr. Rauf Mir is still here—because the people
he worked with and admired invited him to stay for just a year or so longer
. . . and because of his faith. He was determined to build the first mosque
in Kansas City despite his knowledge that there were maybe all of five
Muslim families in the area. That project took much longer than he expected,
and that, and his love of his work, kept him in the area.
“Life just happened,” he laughs. He became a citizen in the
‘80s, and it was clear he was a Kansas City resident for good.
All three of his children were born here; his eldest daughter is a doctor,
a son is at Harvard Law School, and another son is a junior at the University
of Kansas. “I’m glad I stayed,” he says. “Kansas City
is a good place to live.”
Dr. Mir became interested in the kidneys as a specialty of internal medicine
because they involve the whole body—in order to be a good nephrologist,
you have to be a good internist. He likes the intricacies of the kidney
and its complicated physiology—and he wanted to try to master the
difficulties. “You can’t of course,” he says. “But
you can certainly try.” He is also appreciative of the advances in
this relatively recent field including more effective drugs for transplantation
and better machines and drugs for dialysis. He works on the preventative
side as well as early detection.
Dr. Mir has continued his active participation within his faith. There
are now between 7,000 and 10,000 Muslims in Kansas City, and two years
ago he was awarded the Kansas City Interfaith Council Annual Award. He
says it continues to be important “to
reach out to the rest of the community, to know our neighboring faiths,
and to help one another.”
|
 |
|
J. Patrick
Murphy
Pediatric Urologist
For a guy who didn’t know exactly what
he wanted to do almost until he started doing it, Dr. Pat Murphy certainly
does a lot of it. Around 700 surgeries a year, if he were counting—which
he doesn’t. In high school (Shawnee Mission North) and college (the
University of Kansas), what he did know is that he liked the sciences,
especially biology. Going to medical school was a sort of evolution, as
was his interest in surgery. The pediatric part came about because he
worked with two pediatric surgeons he greatly admired, and from there
it was a natural selection.
“I’m manual rather than cerebral,” Dr. Murphy says quietly.
“I see a problem and want to fix it.” He found urology interesting
because there are so many obstructive and reconstruction problems that
affect the entire child. Between one and two percent of children have
some sort of dysfunction, from the simple hernia to the rare case of epispadias
(a urethra abnormality). “While the percentage is not huge, the number
of children who can be helped is,” he points out.
He says he likes the operating, the technical aspects. Recent helpful
changes have included instrumentation and sutures becoming finer and easier
to use. Anaesthetic agents have improved so outpatient care works for
more children. And laparoscopy has made its way into children’s surgery,
which has also helped. Beyond advances, though, his own personality and
drive have helped him maintain a hectic schedule whether he’s at
Children’s Mercy three days a week, KU one day, or his private practice
with six other pediatric surgeons. How does he spend his spare time? Watching
his son’s sports and doing missionary medical work in the Dominican
Republic, where a daughter is now.
What makes the hours and the lack of sleep and all the hard work worthwhile
is seeing a child you can help, he says. “The most fun is working
with kids. They’re innocent and they respond well. The younger they
are, the quicker they get better. The downside is the emotional extremes—the
children you can’t help or correct as much as you want. On the other
hand, you can often help someone for 80 years.”
|
 |
|
Jane
Murray
Family Physician
“I’ve always been intrigued by what
patients tell me has worked. I’ve always listened. And I’ve
discovered there’s much more than just traditional Western medicine
that makes sense.” Dr. Jane Murray is a traditionally trained doctor
who has embraced other remedies from many different cultures. The result
is her Sastun Center of Integrative Health Care, opened in 1998, which
she characterizes as “family medicine with an open mind.”
Sastun is the Mayan word for the amulets the healers used, and it represents
the idea that healing power resides within each person. She believes that
her job is to help people find that healing power, through whatever methods
that work. Consequently, her practice includes more than conventional
Western medicine—it embraces Oriental medicine, massage therapy,
nutrition and Taoist counseling, and more. She counsels patients on healthy
lifestyle, self-care, stress management, natural herbs and vitamins.
This is all a bit of a leap for a woman whose medical degree is from UCLA
and whose background includes stints at the American Academy of Family
Physicians as director of education and then chairwoman of the Family
Medicine Department at the University of Kansas. But she decided that
she wanted to go back to relationship doctoring, not the business transactions
mandated by a health-system plan that she sees as dysfunctional. “Today
we’re forced to see as many patients as possible—get an x-ray,
get a blood test, take a pill. I wanted to go back to the doctor-patient
relationship. And now I’m happy,” she says.
She’s happy despite earning half as much as the typical family physician
and having no benefits. She maintains it’s worth it to have a more
controllable life style and a more personally rewarding practice. She
believes she offers an “old-fashioned doctor relationship with the
latest medical know-how.” She says that, “Technology has become
somehow more important than people, and the fundamental principles we
went into medicine for often seem to be lost. I wanted to try something
new, a true combination of the best of all worlds. I was willing to take
the risks.”
Her message must resonate—she has a three-month waiting list for
new patients.
|
 |
|
Chris
Perryman
Internist
“The number one thing my mentor taught
me was to always listen.” Simple advice, perhaps, but words that
have meant much to Chris Perryman in his chosen career in internal medicine.
“I like working with the whole person,” he states cheerily.
And so, he does a bit of everything in his day, a reason he’s stayed
at St. Luke’s ever since his residency. Daily, he sees patients,
does rounds with residents and medical students, then comes back and sees
more patients. He relishes being a diagnostician, loves the technical
advances in his field, and wants to be informed about everything that’s
going on. In his typical 12-hour day, he enjoys both teaching and his
private practice, saying, “I’m fortunate to have such a good
blend.”
Part of that blend also includes a sincere interest in physicians being
treated fairly. For 13 years he was part of a three-person practice, but
in the last nine years, he has been in a larger medical group at St. Luke’s.
“For physicians to better understand all aspects of our health-care
system, we have to be involved.” Working on numerous health-care
delivery-system activities has given him a different perspective and greater
empathy for all viewpoints. “I think I have a better understanding
of what’s going on in a system where the care is the best, even if
the financial structure is not what it should be yet.”
Another huge part of his good fortune, he says, was marrying his wife,
Kathy. She was a nurse in St. Luke’s ICU when they met 24 years ago
and is now a pediatric anesthesiologist at Children’s Mercy and mom
to four kids, including a set of nine-year-old twins. He’s very clear
that he couldn’t have done what he has without her.
Chris Perryman strikes a stranger as a supremely happy man, one who sees
that himself, as well. Plus, he says, “Kansas City as a medical community
is very fortunate. There are many excellent hospitals and physicians,
and it’s a great place to live. I’ve got the best job in the
world. The best family. I’ve got a true haven in both places. I’m
very, very lucky.”
|
 |
|
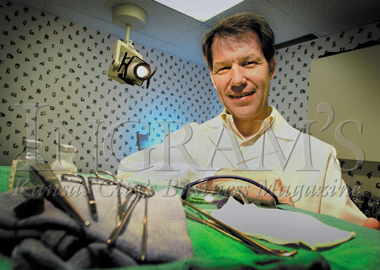
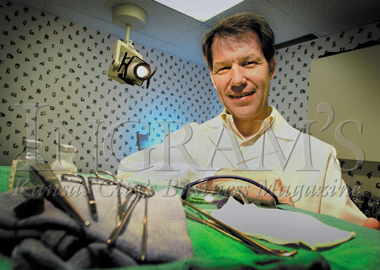
Joseph
Petlein
Laparoscopic Surgeon
The first laparoscopy, done in 1904, used
a scope, a candle and a mirror. Seventy years later, with process and
technology he helped develop, Joe Petelin began telling and showing other
surgeons how laparoscopy could make a huge difference to patients during
and after surgery. He was the first to do abdominal laparoscopy and was
determined that the rest of the world should benefit from what he had
learned. “It’s been most gratifying to see surgeons completely
change their minds once they see the effectiveness of the procedure,”
he declares.
Dr. Petelin was, as he tells it, just your normal doctor. Growing up in
Kansas City, Kan., he earned a bachelor’s degree in physics from
Benedictine College and his medical degree from the University of Kansas.
While lecturing on laser surgery, he met a guy in Nashville who was doing
a form of laparoscopy. At first, Dr. Petelin was skeptical, but then realized
its clear potential. Instead of 10-inch incisions, three inches were maximum.
Instead of a week in the hospital, three days were sufficient. While the
operation was the same, getting there was less traumatic, and thus much
easier on the patient.
Laparoscopy is now an accepted procedure, but the advanced laparoscopy
Dr. Petelin specializes in is another matter. It takes thousands of hours
to become expert at it—and that’s why he has created a yearly
fellowship that he funds with some help from corporations. It’s not
easy; it takes at least a year of concentrated study and practice. And
guidance is absolutely vital—so his specialty is growing very slowly.
Dr. Petelin sees people’s lives as a continuum. “I think in
life, each step prepares you for the next thing. Without understanding
physics, I couldn’t have made all the technical advances. Without
carpentry (his avocation) and my dad, I wouldn’t have learned how
to think on my feet and to do it right the first time. Without my college
truck-driving job, I couldn’t have judged a three-dimensional object
in a two-dimensional mirror as well. Life is usually a progression, and
each step is valuable, even if you don’t know it at the time.”
|
 |
|
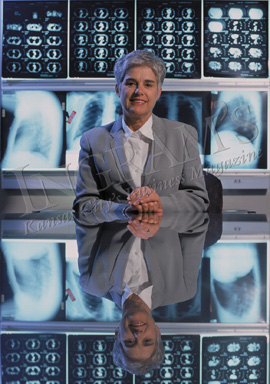
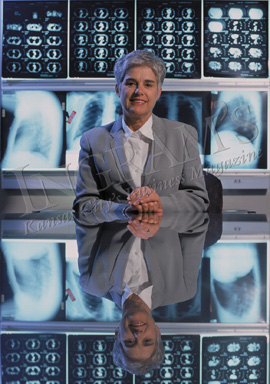
Susan
Pingleton
Pulmonologist
At just 12 years old, Susan Pingleton was
one of the first persons in the world to have open-heart surgery. There
were complications, and she was in the hospital for three months. “People
there literally saved my life,” she remembers. From that time forward,
thinking about becoming a doctor was an easy decision—she wanted
to give back.
Her specialty in pulmonology came about like so many—she had a mentor
who was a pulmonologist and he made it exciting. “We need to be mindful
of our impact on our students,” says this Jayhawker, who is an educator,
researcher, and clinician. As director of the Pulmonary and Critical Care
Division at the University of Kansas Medical Center since 1992, she still
loves her job. “I can do so many things—educate, do procedures,
research, lecture, and see patients. My life is never boring or routine.”
She is especially fond of a teaching hospital’s capability of educating
students while delivering the very best of care to patients.
One of the biggest changes she’s encountered in over 20 years in
academic medicine (she began the pulmonary division for UMKC, where she
was for five years before KU) is that medicine has become a business,
grounded in reality. “We now have to face what private doctors always
have. It’s an alien culture to us, but we’re learning to be
businesspeople as well as doctors. This is a huge problem in every academic
center in the country—but we are making progress.”
She says that becoming president of the largest clinical pulmonary organization,
the American College of Chest Physicians, has been one of the most important
and rewarding opportunities of her career. Representing the organization,
she was able to advance the causes of prevention and care, “ a good
extension of what I do daily taken to national and international levels.”
The scared young girl in the hospital clearly pursued the right dream.
Dr. Pingleton concludes, “I enjoy my life, my family, my terrific
husband, my outside activities. I have a job I love, and I hope I’m
making a valuable contribution.” It would be hard to hope for more.
|
 |
|
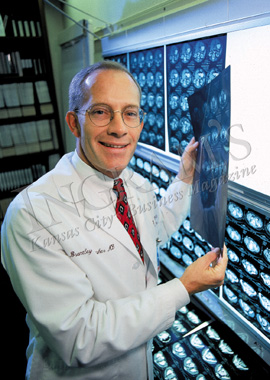
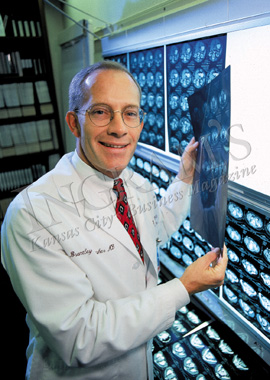
Stephen
Reintjes
Neurosurgeon
“What’s a good day? A good day for
me is when all my operative cases are going well and I can even get home
in time for dinner with my wife and (five) kids.” Between work and
family, the days and nights are full for Dr. Steve Reintjes of the Kansas
City Neurosurgery Group.
Dr. Reintjes, a Rockhurst graduate before college at Georgetown, majored
in philosophy. That study taught him he wanted a field in which he could
care for people. Medicine provided that. The neurosurgery interest came
about during his internship at St. Luke’s because, he says, it’s
precise, high risk, and intellectually challenging (which may be why there’s
only 3,000 neurosurgeons out of 550,000 doctors). After completing his
residency at
KU Medical Center, he started out in solo practice, went to a two-man
office, and then merged to form his current organization, the largest
one in Kansas City and one that works with five different hospitals. “I
do think we’ve assembled a group of good people doing good work for
Kansas City,” says Dr. Reintjes. “Our goal is simply to serve
the community as best we can.”
He’s enthusiastic about the changes that have occurred in the field.
“Today we can treat lesions and diseases safely we couldn’t
touch 10 years ago,” he says. But the part of neurosurgery he likes
the best is meeting patients, getting to know them, and taking care of
them in a time of need. He’s confident even greater advancements
will occur in treating very difficult diseases such as Parkinson’s
and potentially Alzheimer’s, which he says is more vexing than we
can imagine. He summarizes, “The brain remains elusively fascinating.”
Dr. Reintjes does not speak easily about himself, but when pushed, admits
that, besides his kids, he’s proud of his neurosurgery group. A member
of both the Brain Injury Association and the Midwest Organ Bank boards,
he also can’t underscore enough the importance of organ donation.
Since demand still far outstrips supply in organ donation, he calls it
“a generous and life-saving gift.” He’s as determined to
continue working for these important causes as for his patients.
|
 |
|
J. Brantley
Thrasher
Urologic Oncologist
You would have to say that Brant Thrasher
has always been goal oriented. He wanted to go to medical school, so he
had to graduate from college with highest honors. He did. He couldn’t
pay for medical school, but the Army provided scholarships. He got one.
He wanted to study urologic oncology. A fellowship to Duke University
Medical School was the answer. He wanted to be a department chairman (once
he’d finished military obligations) and would need lots of credentials.
Consequently, he wrote, lectured, and researched aggressively.
So at age 37, when he became chief of urology at KU Medical Center, he’d
reached yet another goal–one that he’s still very happy with.
He enjoys the
combination of duties and says figuring out the best part is hard. He
concludes that, “It’s the patients. Helping them recover. There’s
nothing more rewarding than seeing someone healed of cancer.” But
he also enjoys the teaching because, in part, “It keeps me sharp
since I’m working with some very bright residents.” And then
there’s the operating, which he likes because his large reconstructive
cases require skill and precision. To add to these joys, after living
in many places, he and his family really love Kansas City.
Dr. Thrasher points out that of the 200,000 men diagnosed with prostate
cancer each year, 84 percent will live to die of old age or another disease.
Survival rates are improving due to early detection and improved surgical
techniques. But beyond these improvements, when he operated on his father-in-law
10 years ago for the disease, the human lessons came crashing home. “When
it becomes personal, it’s even more real. I try to carry that realization
with me for all my patients.”
When asked what other people might say about him, he laughs and shakes
his head. Finally: “I hope my patients would say I’m compassionate
and caring. I hope the good people I work with would say I’m an excellent
teacher and mentor. I hope the school would say I’m growing a successful
and world-class facility. If they were all saying those things, then that
would be success.”
|
 |
|
Joseph
Waeckerle
Emergency Medicine
“I know it sounds corny, but when I became
a physician, I could help a few people to the best of my ability. When
I became a teacher, I could help other young physicians help them. When
I became editor of a medical journal, I could affect an entire profession—35,000
emergency physicians—and thus, their patients. As I become more and
more involved in emergency awareness on the national basis, I am affecting
even more people. The sacred trust is magnified as you try to be the best
you can for more and more people.” Joe Waeckerle speaks from the
heart.
For the last 30 years, his whole life has revolved around emergency medicine.
He says its great challenge is that you can be faced with a life-threatening
event as well as a minor one simultaneously, and you need to provide full
care to both.
He has become one of the world’s experts on medical preparedness
for weapons of mass destruction including bio-terrorism. He was in charge
of rescue triage at the Hyatt disaster and has spent the last eight years
consulting with the Department of Justice. He’s been especially busy
since Sept. 11th—a pattern he expects will continue. He’s also
always been involved in sports, volunteering his services at clubs and
high schools. He works for the Chiefs, he’s the chair for four hospitals’
emergency-care departments, he’s president of his 40-doctor practice,
he coaches his son’s sixth-grade football team, and he attends activities
of all three at-home sons.
Dr. Waeckerle, a thoughtful and expressive man, finds it “disheartening
that we live in the greatest country in the history of mankind, and we
can’t seem to provide health care for 40 million of our people. We
spend time focusing on issues that don’t improve our country. We’ve
forgotten to ask what we can do for our country.” He continues, “I
feel fortunate to be able to do my part. And that my colleagues also all
feel that we have this same sacred trust of medicine to do all we can,
to do the best we can.”
|
 |
| |
|